Choosing the right palliative care is important for patients and their families. It can significantly impact the quality of life during a difficult time, providing comfort, relief, and support.
In this article, we’ll explore the importance of selecting the right palliative care and share some practical tips to help you make an informed choice. Let’s start by understanding the pivotal role palliative care plays in the lives of patients and their loved ones.
What is Palliative Care?
Before diving into the tips for choosing the right palliative care, let’s take a moment to understand what it is and why it’s so important. Palliative care is a specialized medical approach that focuses on relieving the symptoms, pain, and stress of a serious illness. It aims to improve the quality of life for both the patient and their family, addressing their physical, emotional, social, and spiritual needs.
In essence, palliative care is a supportive and compassionate service that works alongside the patient’s medical treatments, ensuring they receive the best possible care during their illness. It can be beneficial at any stage of a serious illness, not just in the final stages of life. Now that we have a clear understanding of palliative care, let’s discuss how to choose the right one for your needs.
Factors to Consider When Choosing Palliative Care
Selecting the right palliative care for yourself or a loved one can be challenging. To make this process easier, we have compiled a list of factors to consider when making your decision. Keep in mind that the goal of palliative care is to provide comfort and improve the quality of life for those with serious illnesses.
Assess Your Needs
Before you start looking for palliative care options, it’s essential to evaluate the patient’s specific needs. Consider their physical, emotional, social, and spiritual needs. List their symptoms, medication requirements, and any special care they may need.
Research Available Options
Once you clearly understand your needs, research the different palliative care options in your area. This may include hospital-based programs, home care services, or specialized facilities. Gather information on their services, staff, and reputation.
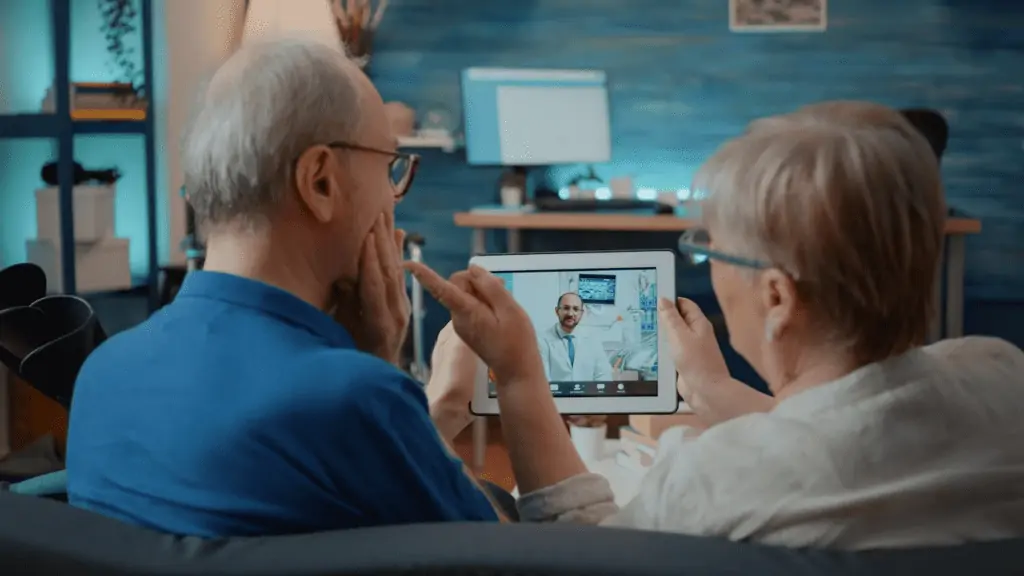
Consult Your Healthcare Team
Your healthcare team can be a valuable resource in finding the right palliative care. They can provide recommendations based on their experience and knowledge of local options. Don’t hesitate to ask for their input and guidance.
Evaluate the Quality of Care
It’s crucial to ensure the chosen palliative care provider offers high-quality care. Look for accreditations, certifications, and professional affiliations. Additionally, read online reviews and testimonials to get an idea of other patients’ experiences.
Meet the Palliative Care Team
Schedule a meeting with the palliative care team to discuss your needs and expectations. This will also give you an opportunity to evaluate their communication skills, empathy, and professionalism. Make sure you feel comfortable and confident in their ability to provide the care you need.
Consider the Cost
Palliative care costs can vary depending on the type of services and the provider. Make sure to inquire about the cost and payment options, as well as any insurance coverage or financial assistance programs that may be available.
Location and Accessibility
Choose a palliative care provider that is conveniently located and easily accessible for both the patient and their family. This will make it easier for loved ones to visit and provide support during this difficult time.
By considering these factors, you can make an informed decision and find the right palliative care provider to meet your needs and ensure the best possible quality of life for you or your loved one.

Why Choose EG Healthcare for Palliative Care
When it comes to choosing the right palliative care provider, EG Healthcare stands out as a top choice. Our dedicated and compassionate team is committed to providing the best possible care for patients with serious illnesses. Here’s why EG Healthcare should be your go-to option for palliative care:
Personalized Care Plans
At EG Healthcare, we understand that every patient is unique, and so are their needs. Our team works closely with patients and their families to create personalized care plans that address their specific physical, emotional, social, and spiritual needs.
Expertise and Experience
Our palliative care team is made up of highly skilled and experienced professionals, including physicians, nurses, social workers, and spiritual counselors. They have extensive training in palliative care and are dedicated to providing the best possible care for our patients.
Comprehensive Support
We believe in a holistic approach to palliative care, which means we offer comprehensive support for patients and their families. This includes managing symptoms, providing emotional and spiritual support, and coordinating care with other healthcare providers.
Accessible and Convenient Location
Our palliative care center is conveniently located, making it easy for patients and their families to access our services. We also offer home-based palliative care for those who prefer to receive care in the comfort of their own homes.
Transparent Pricing and Insurance Support
We understand that the cost of palliative care can be a concern for many families. At EG Healthcare, we offer transparent pricing and work with various insurance providers to help make our services more accessible and affordable.
Exceptional Reputation
EG Healthcare has earned a reputation for excellence in palliative care. Our patients and their families consistently praise our team for their compassion, professionalism, and commitment to providing the highest quality care.
Choosing EG Healthcare for palliative care means you’ll receive the best possible care and support during this challenging time. We are dedicated to improving the quality of life for our patients and their families, ensuring they can focus on what matters most.
Making the Right Choice for Comfort and Support
Choosing the right palliative care provider is a vital decision that can significantly impact the well-being and comfort of patients and their families. By considering factors such as personalized care plans, expertise, comprehensive support, and reputation, you can make an informed choice that best meets your needs.
Take the time to research, consult with healthcare professionals, and evaluate your options. Remember that the right palliative care provider can make all the difference in ensuring comfort, support, and improved quality of life for patients and their families during this challenging time.